Drexler Lab
Molecular Virology & Viral Vector Vaccines
· Ingo Drexler
· Sha Tao
· Ronny Tao
· Guiseppe Andreacchio
· Sarah-Jaqueline Tofan
· Lena-Sophie Wilschrey
· Sebastian Patrick Lohöfer
· Sophie Brügelmann
· Joudi Qasem
Research focus
Our group focuses on the immunobiology of poxviruses and their development and characterization as viral vectors and recombinant vaccines. Working model is the modified vaccinia virus Ankara (MVA) which is a highly attenuated vaccinia virus strain and currently tested as a vaccine vector against infectious diseases and cancer. We are interested to dissect the basic requirements for the efficient induction, expansion and maintenance of MVA-mediated immunity. In particular, we are aiming to characterize the molecular and cellular mechanisms which control and shape the quality and quantity of antigen-specific CD8+ and CD4+ T cell responses during viral infections or vector-based vaccination. This also includes to broaden our knowledge and understanding of virus-host interactions on the molecular level for instance with components of the antigen processing and presentation machinery. Vaccines generated by us are being studied in vitro and in vivo in preclinical animal models as well as in collaborative clinical studies. Our research is directed to develop new approaches for viral vector design, novel vaccine formulations with improved efficacy and optimized preventive and therapeutic MVA-based immunization strategies (e.g. vaccination protocols for T cell-pillowed immunotherapy). Additionally, we are developing diagnostic tools in response to emerging viral diseases such as Mpox.
Viral vector design and vaccine development
The adoption of up-to-date methodology for convenient vector generation, vector quality control, and vector vaccine immune monitoring has increased the pace bringing recombinant MVA vaccines into clinical trials. By now, initial studies testing MVA vaccines for prophylaxis or immunotherapy of infectious diseases and cancer have been completed. First results are overall very encouraging confirming clinical safety, but importantly also demonstrating first clinical efficacy despite the intrinsic difficulties associated with these target diseases. Moreover, MVA is reconsidered as prime candidate vaccine for safer protection against orthopoxvirus infections. However, knowledge about the biological properties of target antigens or modalities of antigen delivery to efficiently induce or expand MVA-vaccine-mediated immunity in vivo is still sparse. We found that CTL responses against MVA-produced antigens were dominated by cross-priming in vivo, despite the ability of the virus to efficiently infect professional antigen-presenting cells (APC) such as dendritic cells (DC). Moreover, stable mature protein was preferred to pre-processed antigen or antigen fragments as the substrate for cross-priming. These findings demonstrate that MVA vaccine design can be essentially improved, as they point to the need for optimal adjustment of the target antigen properties to the intrinsic requirements of the delivering vector system. Therefore, one focus of our work is the identification of key mechanisms essential for the efficient generation (priming) and expansion (recall) of anti-viral or vaccine-induced T cell responses. Next to the optimization of the vector backbone and expression of target genes, we aim to optimize protocols for generation, isolation and molecular characterization of MVA vector viruses e.g. by using recombinant BAC-technology.
Models for immunoprophylaxis and -therapy
We have established or collaborate on preclinical animal models to test MVA vaccine efficacy for viral (e.g. EBV (MHV68)) or bacterial diseases (e.g. Chlamydia trachomatis) and cancer (malignant melanoma, breast cancer). The quality and quantity of induced immune responses is determined for humoral (ELISA, neutralization assays) and cellular (intracellular cytokine release, multimer binding, in vivo cytotoxicity) immunity with particular emphasis on functional and phenotypical characterization of antigen-specific MVA-mediated CD8+ and CD4+ T cell responses. Our target antigens are structural/non-structural viral (e.g. S-/N-antigen (SARS-CoV-2), ORFs (MHV68), pp65 (HCMV)) or bacterial proteins (CTH522 (Chlamydia trachomatis)), so-called differentiation antigens (e.g. tyrosinase, TRP-2) for melanoma, overexpressed tumor antigens (e.g. HER-2/neu) for breast cancer as well as model antigens (OVA). Our vaccines are evaluated in vaccination studies in a variety of transgenic or non-transgenic mouse models applying direct immunization as well as adoptive transfer protocols.
Immunobiology of poxviruses
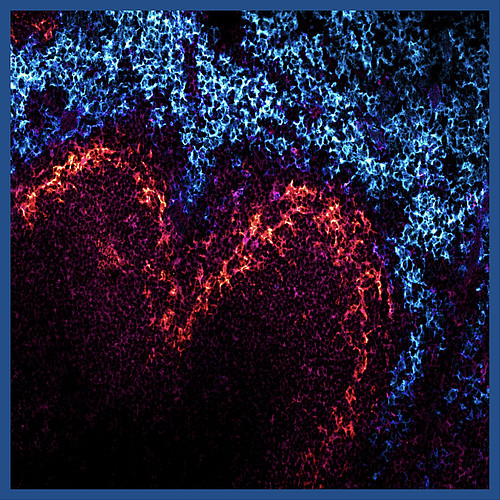
With more recombinant MVA used for antigen delivery in clinical research, there is increasing need to evaluate MVA-specific CD8+ and CD4+ T cell responses following immunization. We identified the first MHC class I (HLA-A*0201)-restricted VACV-epitope which for the first time has permitted comparative T cell analysis for viral vectors and their recombinant target antigens after immunization. Meanwhile, the number of VACV epitopes has been considerably expanded and allowed us to elucidate some of the mechanisms which are relevant for the induction and maintenance of poxvirus-mediated T cell responses in vivo. These include the requirement of cross-presentation of MVA-encoded antigens to efficiently prime naïve T cells as well as the dramatic shaping of the immunodominance hierarchy pattern in the recall or boost vaccination by competing CTL. In this context, we are also studying the role of regulatory T cells for poxviral immunity, the activation pathways for CD4+ T cells or tissue-resident memory T cells, and the impact of the viral life cycle (phases of viral gene expression) on antigen presentation and processing. Additionally, we are investigating the innate immune signalling pathways which are activated during infection or vaccination by viral ligands or molecular patterns and which are directly related to T cell immunity.
The interplay of viral and host mechanisms that regulate the outcome of an infection can result in quite distinct phenotypes for different VACV-strains. The MVA genome lacks functional copies of numerous genes interfering with host response to infection compared to replication-competent VACV strains such as the interferon system or autophagy. We want to use the genetic background information as a comparative basis to characterize the molecular mechanisms associated with these differential phenotypes in vivo. We recently demonstrated that various subsets of DC are efficiently infected by MVA in vitro and in vivo, but fail to induce T cell responses. In particular, late viral antigens are poorly or not processed by infected APC. Next to the interaction of virus and host on the molecular level e.g. within the infected DC, we are addressing systemic questions in the mouse infection model. The identification of distinct APC subtypes which are dominating the induction and expansion of cellular immune responses in primary or secondary poxviral infection and knowledge in which compartments this interplay takes place in vivo, could facilitate novel target-oriented vaccination strategies.



