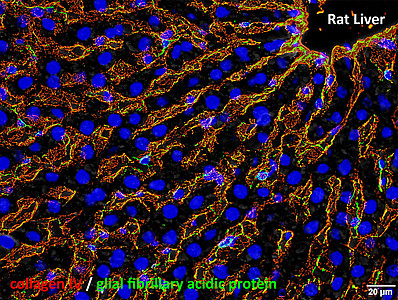
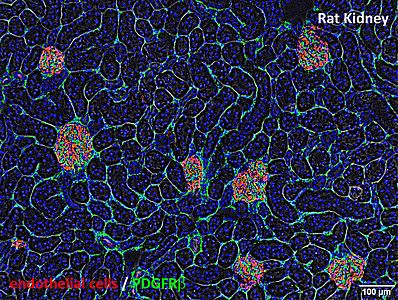
Endothelial cells form blood vessels (red, see images of tissue sections) and thus ensure the supply and function of organs via the bloodstream. Pericytes are in direct contact with the endothelial cells and essentially control their behaviour. Especially on small capillaries that are not covered by a muscle layer, pericytes can be seen through suitable microscopes. Thus, pericytes can be found as so-called hepatic stellate cells on the capillaries of the liver by detecting the protein GFAP (glial fibrillary acidic protein; green) and on capillary networks surrounding the renal tubules by detecting the receptor PDGFRβ (platelet-derived growth factor receptor β; green) (see images of tissue sections).
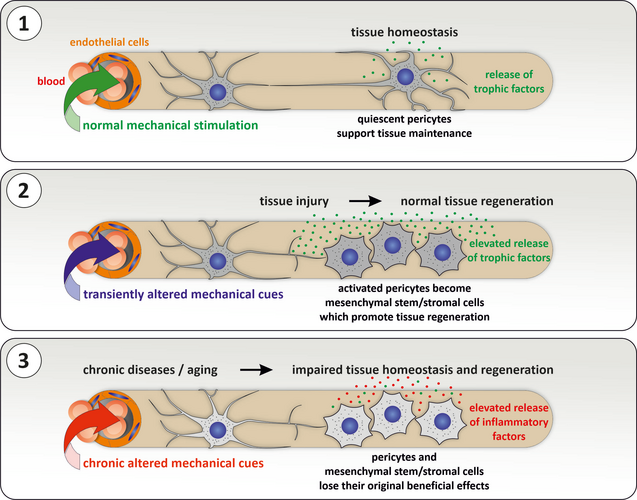
After an injury, pericytes are activated and develop into mesenchymal stem/stromal cells (MSC), which now release more messenger substances or even differentiate into new cell types to support regenerative processes. After tissue regeneration is complete, the MSCs return to a quiescent state as pericytes. To maintain their properties, these adult stem cells require a specific microenvironment called the perivascular stem cell niche. In chronic diseases as well as aging, the microenvironment changes and the adult stem cells successively lose their positive properties and as a result, regenerative processes are impaired. Chronic inflammation also induces increased production of connective tissue proteins (fibrosis), which can lead to impaired organ function and tumour development. It is therefore crucial to better understand the functions and behaviour of pericytes or the MSCs they give rise to in order to develop therapeutic procedures for patients.
The aims of the working group are thus (I) to identify and understand the functions of resting pericytes and activated MSCs in the maintenance and regeneration of organs and (II) to understand the changes in these adult stem cells in chronic diseases and aging. In the long term, these findings should lead to strategies that help to resolve chronic diseases and support regenerative processes of the body. The research focuses primarily on organs such as the liver and kidney, which take into account new approaches to understand physiological processes such as mechanobiology.
Mechanical forces acting on cells include tensile stress and compression as well as shear forces exerted on cells by moving fluids such as blood. The blood flow in the liver and kidney decreases with age and pericytes show clear signs of aging, which are accompanied by a partial loss of function. We have found that mechanical stimulation of pericytes reverses aging processes, so that adequate mechanical stimulation can be seen as an element of their stem cell niche. It also leads to the release of messenger substances from pericytes that are capable of participating in the maintenance of vessels and organs. On the other hand, prolonged and excessive mechanical stimulation of cells, as occurs in chronic liver and kidney diseases, is detrimental and can be seen as a major factor in the development and progression of fibrosis (see schema).
When freshly isolated pericytes of the liver previously loaded with a fluorescent dye are mechanically stimulated by shear forces such as the flow of culture medium a transient influx of calcium into the cells can be detected (red color in the film). This calcium influx activates downstream signaling pathways in the pericytes. We found that there is a rapid release of growth factors to stimulate adaptive or regenerative processes. These results impressively demonstrate the importance of pericytes as adult stem cells for physiological processes, the full extent of which has not yet been fully understood and is of great importance for chronic diseases and the development of therapeutic measures.