Modelling kidney-associated diseases
Bartter and Gitelman Syndrome
This study is in collaboration with the Tubular centre at University College London-UK
https://www.londontubularcentre.org/
Bartter (BS) and Gitelman (GS) syndromes are rare inherited tubulopathies characterized by hypokalaemic, hypochloraemic metabolic alkalosis. They are caused by mutations in at least 7 genes involved in the reabsorption of sodium in the thick ascending limb (TAL) of the loop of Henle and/or the distal convoluted tubule (DCT). BS is a polygenic disease caused by homozygous or mixed heterozygous mutations in one of the genes: SLC12A1-BS1, KCNJ1-BS2, CLCNKB-BS3, BSND-BS4a, CLCNKA, CLCNKB-BS4b and CASR-BS5. GS is an autosomal recessive tubular disorder caused by biallelic mutations in the gene encoding a sodium–chloride cotransporter, SLC12A3 (1).
To date both GS and BS have not been studied using human stem cell-based in vitro models due to the unavailability of relevant cellular models. To overcome this deficit, we employed our previously published protocol to isolate SIX2-positive bipotential renal progenitor cells (UdRPCs) from healthy and patient urine samples of both genders (2). UdRPCs can be differentiated into proximal tubular cells and podocytes with established protocols.
To gain insights into the transcriptomes and associated Gene Ontologies (GOs) and pathways, we carried out bulk NGS comparing undifferentiated UdRPCs from GS, BS2, BS3 and healthy individuals. Cluster analyses of their transcriptomes revealed segregation based on disease states, thus confirming the presence of distinct mutations in GS and BS2, BS3 patients and lack of mutations in healthy individuals.

Prominent biological processes (GO:BP) and KEGG-generated pathways active in healthy cells and compromised in BS2 and 3 patient cells are related to; calcium ion transmembrane transport, calcium ion homeostasis, positive regulation of calcium ion-dependent exocytosis, cellular response to calcium ion, metal ion transport. In addition we see differential expression of members of the Transient receptor potential cation channel family (TRPV4, TRPV1 and TRPA1) which mediate Ca2+ signaling.
Immune-associated pathways were downregulated in BS2 and 3 cells; NF-kappa B signaling, IL-17 signaling, TNF signaling and Leukocyte transendothelial migration.

An inherent feature of UdRPCs is their limited proliferative capacity. To circumvent this, we reprogrammed female and male BS3 cells into iPSCs using our established episomal-based reprogramming protocol (3). We now aim to use these iPSCs together with healthy iPSCs to enhance our meager knowledge of the etiology of BS at the molecular level by comparatively differentiating these into proximal tubular cells (4) for further investigation of the prominent calcium ion-associated biological processes.
1.Sara S Jdiaa , Stephen B Walsh et al (2021). The hypokalemia mystery: distinguishing Gitelman and Bartter syndromes from 'pseudo-Bartter syndrome'. Nephrol Dial Transplant 37(1):29-30.
2.Md Shaifur Rahman et al. (2020). The FGF, TGFβ and WNT axis Modulate Self-renewal of Human SIX2+ Urine Derived Renal Progenitor Cells. Scientific Reports 10: 739.
3. Martina Bohndorf et al. (2017). Derivation and characterization of integration-free iPSC line ISRM-UM51 derived from SIX2-positive renal cells isolated from urine of an African male expressing the CYP2D6 *4/*17 variant which confers intermediate drug metabolizing activity.Stem Cell Res 25:18-21.
4. Isaac Musong Mboni-Johnston et al. (2023). Sensitivity of Human Induced Pluripotent Stem Cells and Thereof Differentiated Kidney Proximal Tubular Cells towards Selected Nephrotoxins. Int J Mol Sci;25(1):81
Investigating the molecular mechanisms underlying APOL1 kidney disease using a unique human urine-derived podocyte cellular model.
This study is with collaborators based at King’s College London
Dr Ania Kozell
https://www.kcl.ac.uk/people/ania-koziell
Dr Kate Bramham
https://www.kcl.ac.uk/people/kate-bramham
Dr Subhankar Mukhopadhyay
https://www.kcl.ac.uk/people/subhankar-mukhopadhyay
People of African descent have a 3-4 times higher risk of chronic kidney disease compared with other ethnicities. This is largely due to the presence of two common protein-altering variants in the Apolipoprotein L1 (APOL1) gene G1 and G2, found exclusively in people of African ancestry. Other populations only express the wildtype (WT) or G0 allele. (1).
Carrying a single high-risk allele (G0/G1 or G0/G2) offers protective benefits against certain infections. However, the presence of two variants, classified as a high-risk genotype (HR; G1/G1, G2/G2, G1/G2), greatly increases the risk of developing kidney disease. The underlying molecular mechanisms remain poorly understood and a “second hit” such as infection (e.g. HIV) or inflammation may be necessary.
Furthermore, APOL1 mediated kidney disease has a phenotypic spectrum, partially dependent on the presence of additional modifying exonic mutations in APOL1. Emerging data from Dr Koziell’s group also supports differences in baseline methylation as another potential mechanism. Importantly, not all HR APOL1 genotype individuals develop kidney disease and this remains unexplained.
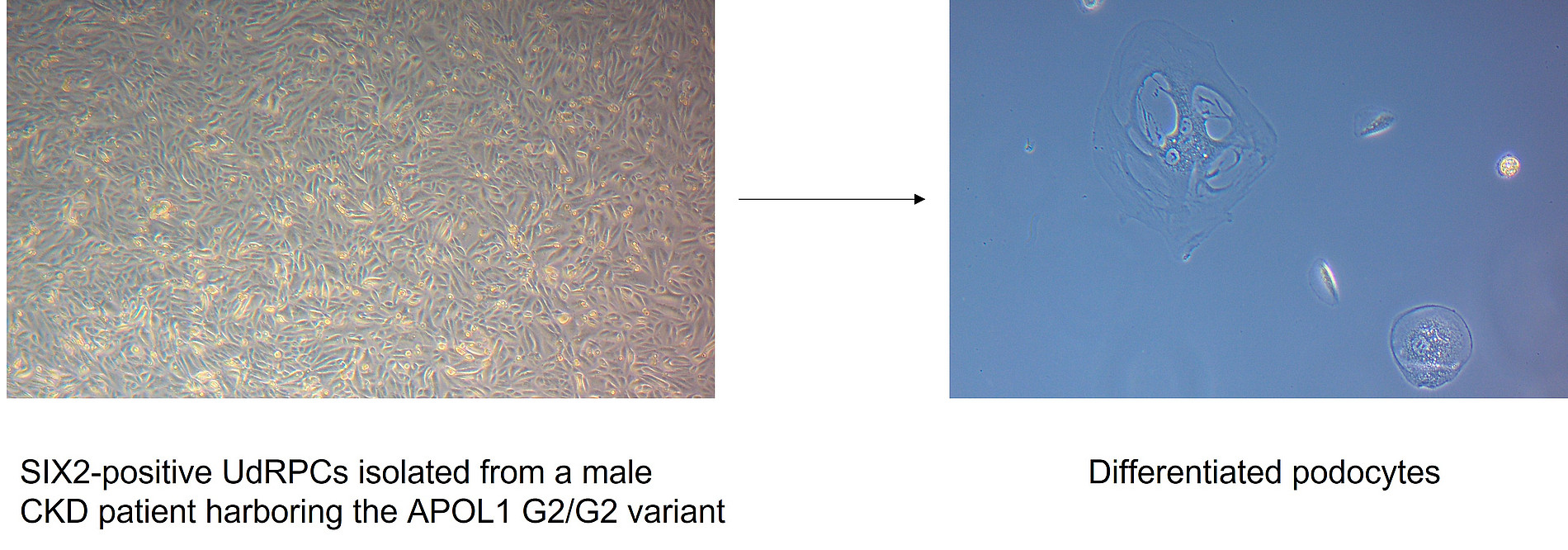
The main target for cellular damage in APOL1 mediated nephropathy are podocytes, highly specialized epithelial terminally differentiated cells in the Bowman’s capsule of the kidney. We has developed a unique technique for growing primary podocytes from patient urine to enable study of the molecular mechanisms underpinning podocyte injury in kidney disease. Dr Koziell’s group have also gathered a unique cohort of 500 patients of African descent (APPLE-CKD) locally at KCL supporting the study and have an immortalised podocyte cell lines to verify findings.
Aims
Urine samples from G0/G0, G1/G1 and G2/G2 individuals with and without CKD will be comparatively analysed for indicator of kidney injury
We apply our published protocol for isolating SIX2-positive UdRPCs from patient (G1/G1) and (G2/G2) urine and further derivation of iPSCs.
Comparative differentiation of UdRPCs and iPSCs into podocytes and the effect of stimulation with pro-inflammatory proteins are investigated at the molecular level
In our previous study, we used a kidney injury-specific assay to assess biomarkers in the urine of healthy individuals and CKD patients (2).

CKD biomarkers identified on the Human Kidney Biomarker Array
(A) Experiments cluster heterogeneously based on the global kidney cytokine expression.
(B) Heatmap and (C) barplot of biomarkers in males
Up-regulated: ADIPOQ, AG, ANXA5, CCN1, FABP1, IL10, LCN2 / NGAL, MMP9, RETN, SERPINA3, TNFA, TNFSF12 and VEGF
Down-regulated: AGER, AHSG, ANPEP, CLU, CXCL16, MME and RBP4.
(D) Heatmap and (E) barplot of biomarkers in females
Up-regulated: AG, AHSG, CLU, IL1RN, MME, RETN, TNFSF12 and VCAM1.
Down-regulated: ADIPOQ, AGER, ANPEP, ANXA5, CCL2, CCN1, EGFR, IL6, MMP9, PLAU and VEGF.
LCN2/NGAL and CLU are well established biomarkers of acute kidney injury/AKI and CKD
Comparative secretion of pro- and anti-inflammatory cytokines from urine derived from healthy and CKD patients

CKD-associated inflammatory biomarkers identified using a human XL cytokine assay
(A) Data cluster into CKD and healthy control based on global cytokine expression. (B) Heatmap and (C) barplot of markers in males (M) that were up-regulated (up) or down-regulated (down). (D) Heatmap and (E) barplot of markers in females (F) that were up-regulated (up) or down-regulated (down). Markers in experiment series 3 that overlapped between females (F) and males (M) that were up-regulated in CKD: APOA1 (up), ANGPT2 (up), C5 (up), CFD (up), GH1 (up), ICAM1 (up), IGFBP2 (up), IL8 (up), KLK4 (up), MMP9 (up) and SPP1 (up).
1. APOL1 Bi- and Monoallelic Variants and Chronic Kidney Disease in West Africans (2025). H3Africa Kidney Disease Research Network N Engl J Med 392:228-238
2. Wasco Wruck, Vincent Boima, Lars Erichsen, Chantelle Thimm, Theresa Koranteng, Edward Kwakyi, Sampson Antwi, Dwomoa Adu, James Adjaye (2020). Urine-Based Detection of Biomarkers Indicative of Chronic Kidney Disease in a Patient Cohort from Ghana. J Pers Med 13.


