AG Lüdde
Research
Hepatocellular carcinoma (HCC) is the most common form of liver cancer and is a leading cause of cancer-related deaths worldwide. In most instances, HCC arises in the setting of chronic inflammation and subsequent liver cirrhosis. While the number of patients with liver cancer is increasing worldwide, only a minority of patients can currently be cured. This is mainly due to the lack of understanding of the pathogenesis of inflammatory liver diseases, which manifest themselves via chronic liver injury into liver cancer development. Our goal is to develop novel drugs and therapeutic options for the treatment of acute and chronic liver diseases and liver cancer. In this regard, we focus on the following three aspects of liver research, which include basic research projects in genetically modified mice and cell culture systems as well as more clinically oriented projects in patient-derived organoids and patient cohorts treated in our clinic. In all three topics, we currently have free positions for medical students that want to do their medical thesis as well as for scientist (Master, PhD thesis, Postdoc). We are collaborating with several groups in the US and Europe.
Role of inflammatory signalling pathways and cell death in the developemnt of acute-, metabolic liver disease and liver cancer
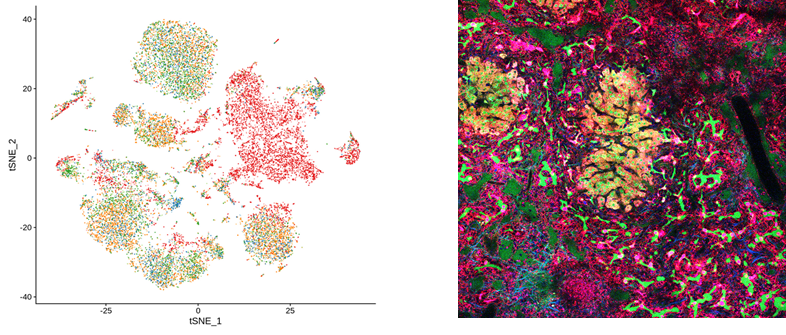
The occurrence of cell death represents a key event in all chronic liver diseases, but it has not yet been elucidated how cell death and inflammation are associated with the malignant transformation of hepatocyte. For many years, our group has focused on the role of pro-inflammatory signaling pathways down-stream of the TNF receptor (TNF-R1) in the context of acute liver damage (Paracetamol intoxication), metabolic liver disease such as alcoholic steatohepatitis and non-alcoholic steaotohepatitis (ASH and NASH) and liver cancer. Our focus is to investigate the role of different programmed cell death forms (apoptosis, necroptosis, pyroptosis, ferroptosis, etc.) in acute and chronic liver diseases and their unique effects on the inflammatory response that play a role in mediating liver injury, liver fibrosis and carcinogenesis. We use standard immunological and cell biological technologies such as FACS, cell sorting, Electro-Mobility-Shift-Assays, Western Blots, qRT-PCR, immunohistochemistry as well as cutting-edge technologies like Single-Cell RNA Sequencing, two-photon microscopy and artificial intelligence (AI) to study the role of programmed cell death pathways in mouse models, primary cell culture systems, organoids as well as human tissues.
Role of non-coding RNAs in models of liver disease.
For several years, we have been investigating the role and function of microRNAs, small non-coding RNAs involved in the suppression of gene transcription/translation. As such, we have demonstrated a new molecular role of the microRNA-29 family in mediating liver fibrosis and microRNA-193a-5p in the development of hepatocellular carcinoma. Now we are analyzing additional microRNA and other nob-coding RNA (circRNA etc.) and their specific target genes regulating fibrosis, hepatocellular carcinoma as well as cholangiocarcinoma.

Biomarkers and artificial intelligence in the treatment of gastrointestinal tumours.
Deep learning is superior to humans in some areas of medical diagnostics and uses histological or immunohistochemical images to identify specific mutations or is able to predict the survival of tumor patients. With this technology, we try to find out whether it can be used in the future for the early detection of cancer or for predicting treatment successes and outcomes in patients.
For more information see: DEEP LIVER


