Research
Main Research Targets of This Group:
1. Ablation Therapy
2. Device Therapy
3. Neuro-Cardiology
1. Ablation Therapy
Catheter ablation therapy has become a cornerstone therapy for many arrhythmias. To improve the outcome of ablation therapy, various conceptual and technological developments have been accomplished during the last decade or two.
However, the treatments of complex arrhythmia such as persistent atrial fibrillation, atrial tachycardias and ventricular tachycardias remain challenging and time consuming. The main goal of this clinical research group is to establish and evaluate new therapeutic tools and systems in the field of catheter ablation.
1-1. Atrial Tachyarrhythmias
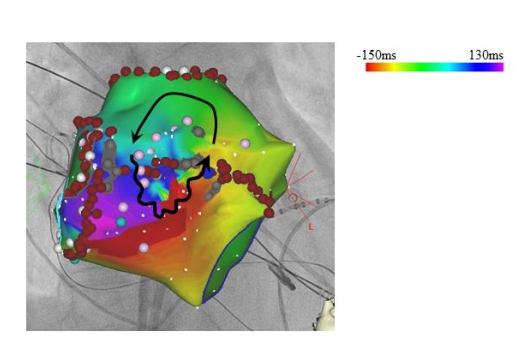
Here we show one case of a left atrial tachycardia. With the detailed mapping in the left atrium a circulating activation around small scar area in the anterior wall of left atrium was identified. After the accomplishment of an “anterior line” with radiofrequency ablation, this tachycardia was terminated and abolished.One goal of this group is to shorten these complex procedures by way of establishing efficient strategy using new developed technologies including 3D-mapping system.
In our group, the cryo-balloon technology has been introduced for atrial fibrillation ablation. The efficient combination of cryo-balloon technology and current 3D-mapping techniques can be a future solution for complex atrial fibrillation.
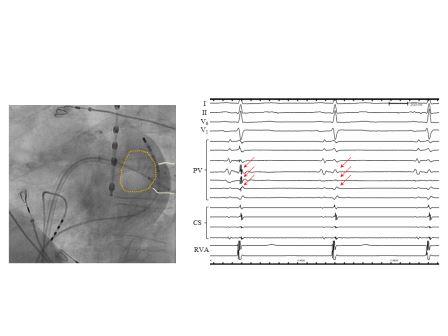
The orange circle is a cryo-balloon, and the left inferior pulmonary vein is well occluded (left panel), resulting in the isolation during the application (right panel, red arrows).
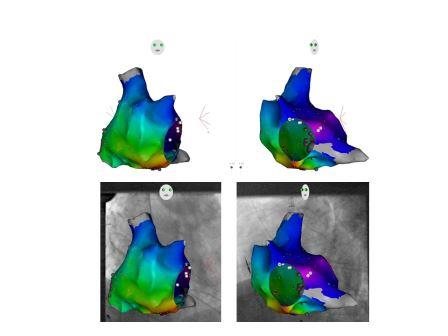
The fluoroscopic reduction is also one of our themes. The introduction of fluoroscopy integration system together with existing 3D-mapping system significantly reduces X-ray exposures. One example is shown below. This patient has a pacemaker (red arrow shows the atrial lead), therefore a careful catheter manipulation is important. In these cases, fluoroscopic exposure tended to be larger to ensure the safe catheter manipulation and to avoid pacemaker lead dislocation.
With utilizing fluoroscopy integration system (panels below), the fluoroscopic reduction is enabled.
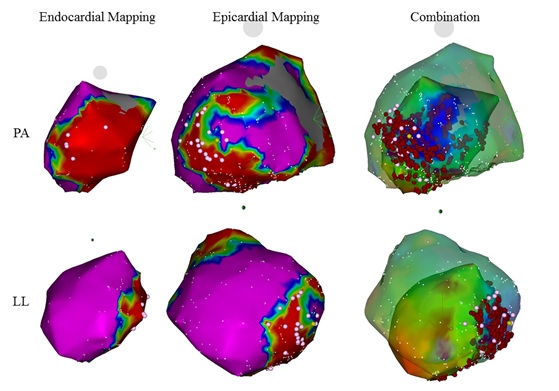
1-2. Ventricular TachyarrhythmiasNow that the catheter ablation for ventricular tachycardias (VT) in patients with structural heart diseases have become a standard procedure to avoid repeated ICD-shocks. The repeated ICD-shocks are already known to make the prognosis of patients worse.For patients with VT and structural heart disease, to make the procedure efficient means to facilitate easier peri-procedural intensive care. However, not only the endocardial ablation but also the epicardial ablation are essential to eradicate arrhythmogenic substrates in these patients' population (figure below).In our group, a novel multipolar catheter and mapping system have been introduced to improve the efficiency and outcomes of the procedures.
2. Device Therapy for Cardiac Arrhythmias
The cardiac device therapy covers a broad range of topics.Of course, the main aims of these therapies are to 1) prevent sudden cardiac death in patients with reduced left ventricular function and 2) avoid bradycardias in patients with cardiac blocks (sick sinus syndrome / atrioventricular block). For these purposes, we are participating in the multicenter studies to develop novel cardiac devices and leads.
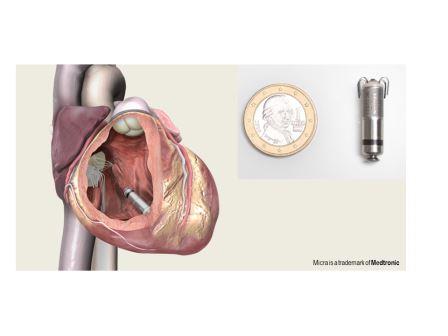
We have started an implantation of novel leadless pacemaker in 2015, as a first center in Germany. This novel pacemaker enables a pure catheter-based implantation, and subcutaneous device implantation or transvenous leads are not any more necessary.
With utilizing insertable cardiac monitor (implantable loop recorder), cardiac rhythm monitoring is enabled, resulting in detection of atrial fibrillation in patients with previous cryptogenic strokes. A cooperation study with the department of neurology is undergoing to screen patients with higher risks for repeated strokes or atrial arrhythmias.

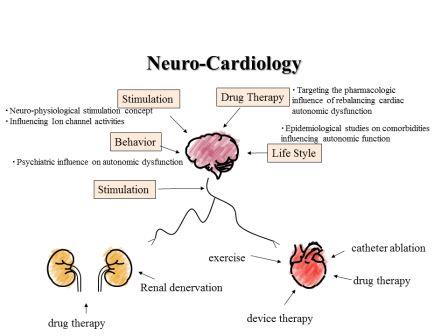
3. Neuro-CardiologyIt has been well known that the cardiac autonomic function plays a great roll in the initiation of cardiac arrhythmias. Moreover, the cardiac autonomic function can predict the prognosis of patients with ischemic heart disease or heart failure.The neuro-modulating devices have been introduced into the clinical practice recently. In cooperation with heart failure unit, and the department of cardiovascular surgery, a neuromodulating therapy targeting heart failure and cardiac arrhythmia has been started.A cardio-renal association is an important inter-discipline topic between cardiology and nephrology. We have published a disturbed autonomic activity in patients with chronic kidney disease. Further studies regarding autonomic-modulation therapy in this field are on-going.

Research Collaboration with the Institute of Neural und Sensory Physiology (Prof. Dr. med. Nikolaj Klöcker)
Project: Arrhythmogenic Mechanisms after Acute Myocardial Infarction: Role of Cardiac HCN-Channels
Myocardial infarction can lead to sudden cardiac death. It is well known that myocardial ischemia is able to generate arrhythmogenic substrates. However, the underlying molecular mechanisms and their time course have not been understood yet.In collaboration with Professor Klöcker and his team, we are trying to clarify the functional role of HCN channels after acute myocardial infarction. This research is a part of the SFB1116 (Master Switches bei kardialer Ischämie).


